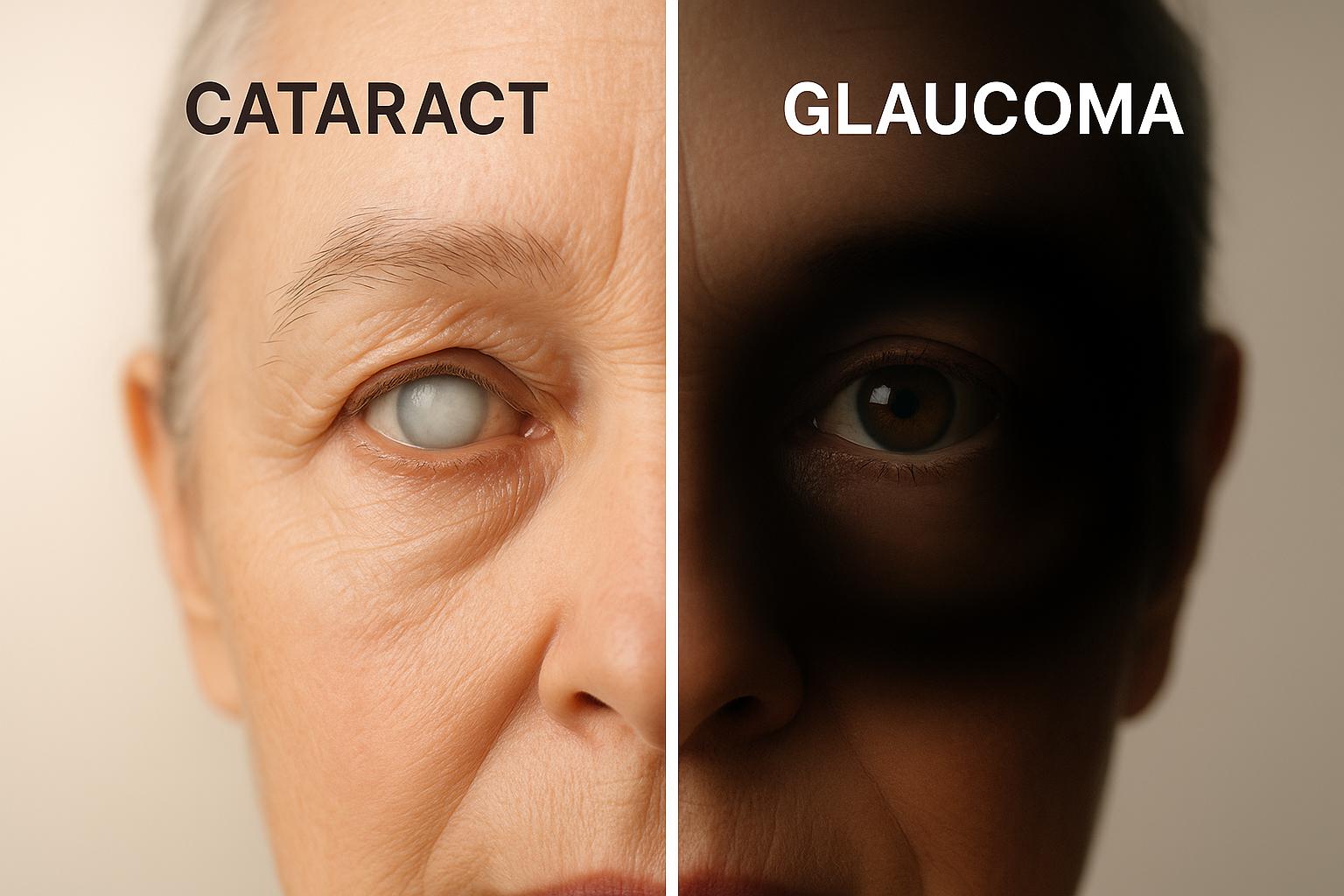
Cataracts and glaucoma are two common eye conditions that can lead to vision loss, but they differ significantly in causes, symptoms, and treatment. Cataracts cloud the eye’s lens, causing blurry vision that can be corrected with surgery. Glaucoma damages the optic nerve, often silently, leading to permanent vision loss if untreated. Regular eye exams are crucial for early detection and effective management.
Key Points:
- Cataracts: Cloudy lens, gradual vision loss, reversible with surgery.
- Glaucoma: Optic nerve damage, often symptomless early on, vision loss is irreversible.
Quick Comparison:
| Factor | Cataracts | Glaucoma |
|---|---|---|
| Affected Area | Lens | Optic nerve |
| Cause | Aging, UV exposure, diabetes, smoking | High eye pressure, aging, family history |
| Symptoms | Blurred vision, glare, trouble at night | Often none early; peripheral vision loss |
| Treatment | Surgery | Eye drops, laser, or surgery to lower IOP |
| Vision Recovery | Fully reversible with surgery | Permanent damage; treatment prevents worsening |
Early diagnosis is key. While cataracts are treatable, glaucoma requires lifelong management to prevent further loss.
What Are Cataracts?
Cataract Definition and Basics
Cataracts happen when the lens inside your eye, which is usually clear, becomes cloudy. This lens is crucial for focusing light onto the retina, and when it loses transparency, it can block or scatter light, making your vision blurry or dim.
This cloudiness occurs when proteins in the lens break down and clump together. While this process often begins around age 40, many people don’t notice symptoms until their 60s or later. Let’s dive into what causes these changes.
What Causes Cataracts?
Aging is the leading cause of cataracts, as the natural breakdown of lens proteins over time leads to clouding. Cataracts become more common as we grow older, affecting just 2% of people aged 40–49 but over 90% of those above 80.
However, other factors can speed up this process. For instance, diabetes significantly raises the risk – people with diabetes are three to four times more likely to develop cataracts before age 65 due to high blood sugar levels affecting the lens. Smoking doubles the risk, as harmful chemicals in tobacco cause oxidative stress in the eye. Excessive alcohol consumption can also contribute by causing nutritional deficiencies and oxidative damage.
Eye injuries are another major factor, with about 65% of eye injuries leading to cataracts later. Prolonged exposure to UV rays, certain medications (like long-term steroid use), high blood pressure, and conditions like uveitis also increase the likelihood of developing cataracts.
Women make up 61% of cataract cases in the U.S., and African American and Hispanic populations face higher risks compared to Caucasians.
Cataract Symptoms and How They Progress
Cataracts develop slowly and without pain, so symptoms often go unnoticed until the condition worsens.
"You might not have any symptoms at first, when cataracts are mild. But as they grow, cataracts can cause changes in your vision." – National Eye Institute
Early signs include slight blurriness, increased sensitivity to glare, trouble seeing in dim light, or colors appearing slightly yellowed. Many people first notice issues with tasks like night driving.
As cataracts progress to the intermediate stage, vision becomes noticeably blurry or cloudy. Colors may seem faded, reading or close-up tasks get harder, and glare or halos around lights become more bothersome. Some may even experience double vision in one eye. At this point, frequent updates to eyeglass prescriptions might be needed.
In the mature stage, cataracts can severely impair vision, making everyday activities – like driving, reading, or recognizing faces – extremely difficult. The lens might take on a milky white or brownish tint, becoming visibly cloudy.
In the hypermature stage, cataracts can lead to significant vision loss or even blindness. The lens becomes dense, may shrink and harden, and complications such as inflammation or increased eye pressure can arise.
How Cataracts Are Treated
The good news is that vision loss caused by cataracts can be completely reversed through surgery. Cataract surgery involves removing the cloudy lens and replacing it with a clear artificial lens, known as an intraocular lens (IOL).
This procedure is one of the most common and successful surgeries in the U.S. It typically takes less than 30 minutes, is performed on an outpatient basis, and uses local anesthesia. During the surgery, the surgeon makes a small incision, breaks up the cloudy lens with ultrasound waves (a process called phacoemulsification), removes the fragments, and inserts the artificial lens.
Most people notice a significant improvement in their vision within days to weeks after surgery. In the early stages of cataracts, doctors might suggest managing symptoms with stronger lighting, anti-glare sunglasses, or updated eyeglass prescriptions. But once cataracts start to impact daily life, surgery becomes the only definitive solution.
What Is Glaucoma?
Glaucoma Definition and Basics
Glaucoma refers to a group of eye conditions that harm the optic nerve – the vital connection between your eye and brain. Unlike cataracts, which cloud the eye’s lens, glaucoma directly damages the nerve responsible for transmitting visual information. This damage often happens when the pressure inside the eye, known as intraocular pressure (IOP), gets too high. However, glaucoma can also occur even with normal eye pressure. What makes this condition particularly concerning is that any vision loss caused by glaucoma is permanent – it cannot be recovered.
Glaucoma is the second-leading cause of blindness worldwide, impacting over 3 million people in the U.S. alone. Even more concerning? Up to half of those affected in the United States may not even realize they have it. That’s why glaucoma has earned the nickname "the silent thief of sight." Below, we’ll explore the main risk factors that contribute to this condition.
What Causes Glaucoma?
Age is one of the most significant risk factors for glaucoma. In fact, about 10% of individuals aged 75 and older are affected. A family history of glaucoma also raises your chances of developing the condition. Ethnicity plays a role as well – Black individuals are 15 times more likely to experience blindness from primary open-angle glaucoma, while people of Asian and Inuit descent face a greater likelihood of developing angle-closure glaucoma.
Other health conditions, such as diabetes and high blood pressure, can further increase the risk. Eye injuries can lead to secondary glaucoma, which is why wearing protective eyewear during sports or hazardous work is so important. Additional factors include prolonged use of corticosteroid medications, severe nearsightedness, and having thin corneas. Some individuals are also born with higher-than-average eye pressure (ocular hypertension), which requires monitoring to prevent glaucoma from developing. These factors highlight the subtle and often stealthy progression of glaucoma.
Glaucoma Symptoms and How It Progresses
Primary open-angle glaucoma is known for its quiet progression. By the time noticeable vision changes occur, the optic nerve may already be significantly damaged. Early signs often include a gradual loss of peripheral (side) vision, which can narrow your overall field of view. On the other hand, angle-closure glaucoma develops rapidly and is considered a medical emergency. Symptoms include severe eye pain, sudden blurred vision, intense headaches, nausea, vomiting, and seeing rainbow-colored halos around lights. If you experience these symptoms, seek immediate medical attention, as vision loss can happen within hours.
Some people may also notice subtler changes, such as difficulty adjusting to dim lighting, frequent changes in prescription glasses, or occasional eye discomfort. These signs should not be ignored, as they could indicate early stages of glaucoma.
How Glaucoma Is Treated
The main goal of glaucoma treatment is to reduce intraocular pressure and protect the optic nerve from further damage. While treatments can slow or stop the disease’s progression, they cannot restore lost vision.
"The main difference is that surgery for cataracts can restore vision, whereas the damage caused by glaucoma is permanent." – Victoria Rohring, DO, MS, Ophthalmologist, Eye Institute, Northwell Health
Eye drops are often the first line of defense, working to lower eye pressure by either reducing fluid production or improving fluid drainage. For additional support, laser treatments like selective laser trabeculoplasty (SLT) help enhance fluid outflow. For angle-closure glaucoma, a laser peripheral iridotomy creates a small opening in the iris to improve fluid flow.
If these methods aren’t enough, surgical options may be necessary. Procedures like trabeculectomy create a new drainage channel for fluid, while minimally invasive glaucoma surgeries (MIGS) offer less invasive alternatives with quicker recovery times.
Detecting glaucoma early and sticking to a treatment plan are essential for managing this condition. Since optic nerve damage is irreversible, identifying glaucoma before symptoms become noticeable offers the best chance to protect your vision. Early diagnosis is just as critical as it is for cataracts – it’s the key to preserving your sight.
Cataracts vs Glaucoma: Direct Comparison
Key Differences Between Cataracts and Glaucoma
Cataracts and glaucoma may both impact your vision, but they are entirely different conditions that affect separate parts of the eye. Knowing how they differ can help you spot symptoms early and get the right treatment.
The biggest difference lies in reversibility. Cataracts cause vision issues that can usually be corrected with surgery, while glaucoma damages the optic nerve permanently, making early detection critical. Once vision loss occurs with glaucoma, it cannot be regained.
Here’s a quick breakdown of how these two conditions compare:
| Factor | Cataracts | Glaucoma |
|---|---|---|
| Affected Eye Part | Clouding of the natural lens | Damage to the optic nerve |
| Primary Causes | Aging, UV exposure, diabetes, smoking, eye injuries | High eye pressure, aging, family history, ethnicity, diabetes |
| Early Symptoms | Blurred or cloudy vision, glare issues, trouble seeing at night | Often no symptoms early on ("silent thief of sight") |
| Vision Loss Pattern | Central vision becomes cloudy and dim | Gradual loss of peripheral vision |
| Progression Speed | Develops slowly over years | Open-angle: slow; Angle-closure: rapid onset |
| Pain Level | Typically painless | Open-angle: painless; Angle-closure: can cause severe pain and headaches |
| Treatment | Surgery to replace the cloudy lens | Eye drops, laser treatment, or surgery to reduce eye pressure |
| Vision Recovery | Vision is often fully restored with surgery | Vision loss is permanent; treatments aim to prevent further damage |
| Prevention | UV protection, healthy habits, regular eye exams | Prevention isn’t possible, but early detection can slow progression |
Another key difference lies in symptom timing and treatment urgency. Cataracts generally cause noticeable vision changes early on, giving you time to address the issue when it starts affecting your daily life. Glaucoma, on the other hand, often progresses quietly until significant damage has occurred. In cases like angle-closure glaucoma, immediate medical attention is necessary to avoid permanent vision loss.
Both conditions become increasingly common as we age, making regular, comprehensive eye exams a vital part of protecting your vision. Early detection can make all the difference in managing these issues effectively.
Cataract vs Glaucoma – What’s the Difference?
sbb-itb-c87b093
How These Conditions Are Diagnosed and Treated
Understanding the diagnosis and treatment of cataracts and glaucoma highlights the critical differences between the reversible vision loss caused by cataracts and the permanent damage from glaucoma.
Diagnosing Cataracts and Glaucoma
Accurate diagnosis plays a vital role in protecting your vision. Eye doctors use a variety of tests to identify these conditions, often during a single comprehensive eye exam.
Cataract diagnosis begins with a visual acuity test, where you read an eye chart to measure how clearly you see at different distances. Your doctor will then perform a dilated eye exam, which involves widening your pupils to examine the lens for cloudiness. A slit-lamp exam provides a detailed, magnified view of your eye’s structures, making it easier to detect cataracts and assess their severity. Additional tests may evaluate how well you see in bright light or how sensitive you are to glare – both common signs of cataracts.
Glaucoma diagnosis requires more specialized testing since it often develops silently without early symptoms. Tonometry is used to measure intraocular pressure (IOP), with normal readings typically ranging from 12 to 22 mmHg. However, glaucoma can occur even with normal pressure levels. During a dilated eye exam, your doctor will also examine the optic nerve for changes like cupping, which can indicate glaucoma. Advanced imaging techniques, such as optical coherence tomography (OCT), measure the thickness of retinal nerve fibers to detect early signs of damage. Visual field testing maps your peripheral vision to identify blind spots that may signal glaucoma.
Timing is critical. Cataracts usually become noticeable to patients as they progress, but glaucoma can cause irreversible damage before symptoms appear. To catch these conditions early, the American Academy of Ophthalmology advises adults over 40 to have comprehensive eye exams every one to two years, with annual exams for those at higher risk.
Treatment Plans for Both Conditions
The treatment strategies for cataracts and glaucoma differ significantly, reflecting the nature of each condition. Knowing these differences can help you understand what to expect and why timely care is essential.
Cataract treatment is straightforward and involves surgery when the condition begins to interfere with daily activities. There are no medications or eye drops to reverse cataracts. Cataract surgery, performed through a procedure called phacoemulsification, replaces the cloudy natural lens with an artificial intraocular lens (IOL).
The timing of surgery depends on how much cataracts affect your quality of life. Some people manage well with mild cataracts for years, while others may need surgery sooner if their vision problems interfere with tasks like driving or reading. Modern cataract surgery often restores vision to levels better than before the cataracts developed, especially with advanced IOLs designed to correct issues like astigmatism or presbyopia.
Glaucoma treatment, on the other hand, focuses on preventing further damage since lost vision cannot be regained. The primary goal is to lower eye pressure, starting with prescription eye drops. These medications fall into different categories, such as prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors, and work by either reducing fluid production or improving fluid drainage in the eye.
If eye drops are insufficient, laser treatments like selective laser trabeculoplasty (SLT) may be used to enhance drainage. For angle-closure glaucoma, a laser peripheral iridotomy creates a small opening in the iris to improve fluid flow.
Surgical options include traditional procedures like trabeculectomy, where a new drainage pathway is created, and minimally invasive glaucoma surgeries (MIGS). MIGS can often be combined with cataract surgery, making them particularly beneficial for patients dealing with both conditions.
Treating both conditions simultaneously requires careful planning. Many older adults develop cataracts and glaucoma, and treatment decisions often overlap. For instance, cataract surgery can sometimes reduce eye pressure in glaucoma patients, particularly those with angle-closure glaucoma. In such cases, a combined surgical approach may be recommended to address both issues at once.
The urgency of treatment differs between the two conditions. Cataract surgery can be scheduled based on your readiness and how much the condition bothers you. Glaucoma treatment, however, demands immediate attention to prevent permanent vision loss. Skipping medications or delaying care can lead to irreversible damage.
Ultimately, treatment plans are tailored to your unique needs, considering factors like age, overall health, lifestyle, and the severity of each condition. Regular follow-up appointments are crucial for both conditions – whether to monitor recovery after cataract surgery or to ensure glaucoma treatments are effectively managing eye pressure and preventing further damage.
Prevention and Getting Care at Boulder Eye Surgeons
Why Regular Eye Exams Matter
Regular eye exams are essential for maintaining your vision and catching issues like cataracts and glaucoma early. Detecting cataracts in their initial stages allows you to consider treatment options before they interfere with your daily life. While cataracts can’t be prevented, early diagnosis empowers you to decide the right time for surgery.
Glaucoma, often called the "silent thief of sight", progresses without obvious symptoms, making routine eye exams even more critical. Early detection can help preserve your vision and potentially avoid more complicated treatments down the line.
For adults over 40, comprehensive eye exams are recommended every one to two years. Those at higher risk – due to factors like family history, diabetes, high blood pressure, or previous eye injuries – should schedule annual exams. Boulder Eye Surgeons provides expert care to support this proactive approach to eye health.
Expert Care at Boulder Eye Surgeons
At Boulder Eye Surgeons, early detection is just the beginning. Their team offers customized treatments designed to protect your vision for the long haul. Using advanced technology and a patient-centered approach, they ensure accurate diagnoses and personalized care – all in one visit.
"We utilize state-of-the-art technology to offer comprehensive medical and surgical eye care. Our goal is to provide each patient with personalized care of the highest quality."
For cataracts, Boulder Eye Surgeons provides both traditional and laser-assisted surgical options. Dr. Samuel Long explains the benefits of laser-assisted cataract surgery:
"Laser-assisted replaces the manual use of blades during cataract surgery. Using a computerized high-resolution scanning system, we’re able to customize the procedure to your eye’s unique characteristics. This allows for the removal of a cataract with greater precision, predictability and safety than in traditional cataract surgery."
They also offer a variety of intraocular lens (IOL) options to suit different needs. Choices range from standard monofocal lenses to premium options like Toric, Multifocal, Accommodative, and Extended Depth of Focus (EDOF) lenses. One standout option is the Light Adjustable IOL, which Dr. Long highlights:
"It is the first and only lens that can be adjusted after cataract surgery. Importantly, unlike other cataract surgery, the Light Adjustable Lens lets you preview your vision options before finalizing your choice."
For glaucoma care, the practice provides a full spectrum of treatment options, including prescription eye drops, laser procedures, and advanced surgical interventions. Their expertise ensures you receive the most effective care for your specific condition.
Patient stories reflect the practice’s dedication to individualized care. One patient, Michael L., shared his experience undergoing cataract surgery with Dr. Cuevas. He praised the thorough follow-up and the time Dr. Cuevas spent discussing solutions tailored to his visual needs.
From diagnosis to long-term follow-up, Boulder Eye Surgeons delivers comprehensive, expert care designed to meet your unique vision requirements every step of the way.
Conclusion
Knowing the distinctions between cataracts and glaucoma is key to taking control of your eye health. Cataracts develop gradually, leading to cloudy vision, but they can be treated effectively with surgery. On the other hand, glaucoma is a silent condition that damages the optic nerve, causing permanent vision loss if not addressed early. Since cataract surgery can restore vision while glaucoma damage cannot be undone, regular eye exams are absolutely critical.
Glaucoma often progresses without obvious symptoms until significant harm has already occurred, while cataracts tend to worsen slowly over time. This makes routine, comprehensive eye exams your best defense. Early detection not only prevents most vision issues but also ensures the best possible treatment outcomes.
Expert care plays a vital role in managing these conditions. At Boulder Eye Surgeons, their reputation is built on a commitment to personalized care and thorough treatment plans for both cataracts and glaucoma.
Taking action now can make all the difference. Scheduling regular eye exams and seeking professional care when needed is an investment in your future vision. Don’t wait for symptoms to show up – start prioritizing your eye health today to safeguard your sight for years to come.
FAQs
What are the early signs of glaucoma, and how can I catch it in time?
Glaucoma often begins quietly, with subtle signs like a slow loss of peripheral vision, halos around lights, eye discomfort, headaches, or blurred vision. But here’s the tricky part: in many cases, it progresses silently, showing no obvious symptoms in the early stages.
The best way to catch glaucoma early is by scheduling regular, comprehensive eye exams, which should include dilated eye tests. These exams are especially crucial if you’re at higher risk – this includes individuals over 60, those with a family history of glaucoma, or people managing medical conditions such as diabetes. Early detection through these professional tests is essential for maintaining and protecting your vision.
Can diet and exercise help lower the risk of cataracts or glaucoma?
Yes, living a healthy lifestyle can significantly help reduce the chances of developing cataracts and glaucoma. Regular physical activity is particularly beneficial, as it may help lower eye pressure – a crucial factor in glaucoma prevention. Plus, staying active contributes to overall eye health.
Eating a diet packed with fruits, vegetables, and whole grains is another important step. These foods are loaded with antioxidants and vitamins that help protect your eyes. For instance, leafy greens, citrus fruits, and foods rich in omega-3 fatty acids are known to support good vision and may lower the risk of these eye conditions. Pairing a nutritious diet with regular exercise is a simple yet effective way to promote eye health and enhance your overall quality of life.
Does cataract surgery impact glaucoma treatment if both conditions are present?
Cataract surgery can sometimes lower intraocular pressure (IOP) in individuals with glaucoma, particularly in cases that are mild or stable. This reduction in pressure may allow for a decreased need for glaucoma medications. However, it’s important to understand that cataract surgery by itself does not treat active or worsening glaucoma.
If you have both cataracts and glaucoma, your doctor might suggest a combined procedure to address both conditions at the same time. This method can help achieve better pressure control and support overall eye health. Still, glaucoma often requires continuous treatment and regular monitoring to manage effectively.