Glaucoma is a serious eye condition that can cause irreversible vision loss if left untreated. Often called the "silent thief of sight", it progresses without noticeable symptoms in its early stages. Here’s what you need to know:
- What is glaucoma? A group of conditions that damage the optic nerve, often due to high eye pressure, leading to permanent vision loss.
- Who is at risk? People over 40, those with a family history, African Americans, Hispanics, individuals with diabetes, severe nearsightedness, or past eye injuries.
- Why is early detection important? Glaucoma damage can’t be reversed, but early treatment can slow or prevent further vision loss.
- How is it treated? Options include eye drops, laser therapy, and surgery, all aimed at lowering eye pressure to protect the optic nerve.
- How can you manage it daily? Stick to prescribed treatments, maintain a healthy lifestyle, and schedule regular eye exams.
Glaucoma affects millions worldwide, with many unaware they have it. Regular screenings and consistent care are key to protecting your vision.
Glaucoma: frequently asked questions
What Is Glaucoma and How Does It Affect Vision?
Glaucoma refers to a group of conditions that damage the optic nerve, leading to permanent vision loss if untreated. This damage is often linked to increased intraocular pressure (IOP), which occurs when fluid within the eye doesn’t drain properly. The resulting pressure deforms the lamina cribrosa, a structural part of the optic nerve, injuring nerve fibers and killing retinal ganglion cells.
The most common form, open-angle glaucoma, accounts for over 90% of cases in the U.S. It develops gradually as drainage canals become clogged. Angle-closure glaucoma, on the other hand, happens when the iris suddenly blocks fluid drainage, creating a medical emergency. Other types include normal-tension glaucoma, congenital glaucoma, and secondary glaucomas like neovascular and pigmentary glaucoma, which can result from injuries, illnesses, or certain medications.
The global impact of glaucoma is staggering. Around 60 million people live with vision loss caused by glaucoma, and nearly half of these cases remain undiagnosed. In the U.S. alone, one in 40 adults over 40 experiences vision impairment due to this condition. Now, let’s take a closer look at how glaucoma progresses and affects your vision over time.
How Does Glaucoma Progress?
Glaucoma often advances silently, which is why understanding how it impacts vision is so important. In its early stages, glaucoma primarily affects peripheral vision – the edges of your visual field. Your central vision, which is critical for tasks like reading, driving, and recognizing faces, tends to stay intact at first. This makes it easy to overlook the condition without routine eye exams.
Adding to the challenge, your brain compensates for early vision loss by "filling in" the gaps in your visual field. This trick of the mind can delay awareness of the problem until the damage has become severe. As the disease progresses, blind spots grow and may eventually invade your central vision. By the time you notice symptoms like bumping into objects, trouble seeing in dim light, or difficulty judging depth, the vision loss is often irreversible.
The speed of progression varies depending on the type of glaucoma. Open-angle glaucoma typically advances slowly, over years or even decades. In contrast, angle-closure glaucoma can cause rapid vision loss in just hours or days. Even normal-tension glaucoma, where eye pressure stays within the normal range, can quietly cause damage over time.
Regular eye exams are key to catching glaucoma early, especially as you get older or if you have risk factors. Early detection allows for timely management, potentially preserving your vision for years to come.
Who Is at Risk for Developing Glaucoma?
Knowing your risk for glaucoma is a key step in taking control of your eye health. While anyone can develop this condition, certain factors can significantly increase the likelihood of its onset. Millions of Americans have glaucoma without even realizing it. By identifying whether you fall into a higher-risk group, you can partner with your eye care provider to create a personalized plan for monitoring and prevention. Below, we’ll explore the main risk factors and explain why regular screening is so important.
What Are the Main Risk Factors?
Age is one of the biggest contributors to glaucoma risk. Once you hit 40, your chances of developing the condition begin to climb, and the risk becomes even greater after age 60. This is because aging naturally impacts the eye’s drainage system, making it harder to manage fluid buildup and increasing eye pressure.
Family history matters a lot. If someone in your immediate family – like a parent, sibling, or grandparent – has glaucoma, your risk jumps four to nine times compared to someone without a family history. This suggests that genetics play a role in how the optic nerve reacts to pressure and other stressors.
Ethnicity also influences risk levels. African Americans are particularly vulnerable, with rates six to eight times higher than those seen in Caucasians. They also tend to develop glaucoma earlier and experience more severe vision loss. Hispanic Americans over 60 are also at higher risk, while Asian Americans are more likely to develop angle-closure glaucoma due to the unique structure of their eyes.
Health conditions like diabetes, high blood pressure, and heart disease can increase the risk by affecting blood flow to the optic nerve.
Severe nearsightedness (myopia) is another factor. Highly myopic eyes often have structural differences that make the optic nerve more prone to damage. The elongated shape of these eyes can thin and stretch the tissues around the nerve, increasing vulnerability.
Past eye injuries or surgeries can also raise the risk. Even injuries from years ago may create scar tissue or structural changes that interfere with normal fluid drainage, setting the stage for glaucoma.
Long-term steroid use – whether through eye drops, pills, or injections – can elevate eye pressure over time. This applies to medications prescribed for conditions like asthma, arthritis, or inflammatory diseases.
Recognizing these risk factors highlights the importance of regular screening.
Why Is Regular Screening Needed?
Glaucoma is often called the "silent thief of sight" because it develops without symptoms in its early stages. Regular eye exams are the only way to catch it early – when treatment can prevent significant vision loss.
How often you need screening depends on your age and risk level. If you’re over 40 and have no other risk factors, getting a comprehensive eye exam every two to four years is usually enough. For African Americans over 40 or anyone over 60, annual exams are recommended because of the increased likelihood of developing glaucoma.
High-risk individuals require closer monitoring. If you have multiple risk factors – like a family history combined with diabetes or severe myopia – your provider might suggest exams every six to twelve months. This frequent monitoring helps detect subtle changes in eye pressure, optic nerve health, or visual field performance that could indicate early glaucoma.
Baseline measurements are incredibly useful. Early screenings establish your normal eye pressure, optic nerve appearance, and visual field patterns. These benchmarks make it easier for your eye doctor to spot even small changes that could signal the onset of glaucoma.
Catching glaucoma early saves money and vision. Advanced cases often require costly treatments, like multiple medications or surgery. In contrast, early detection usually means simple, affordable options – like eye drops – that can protect your vision for years to come.
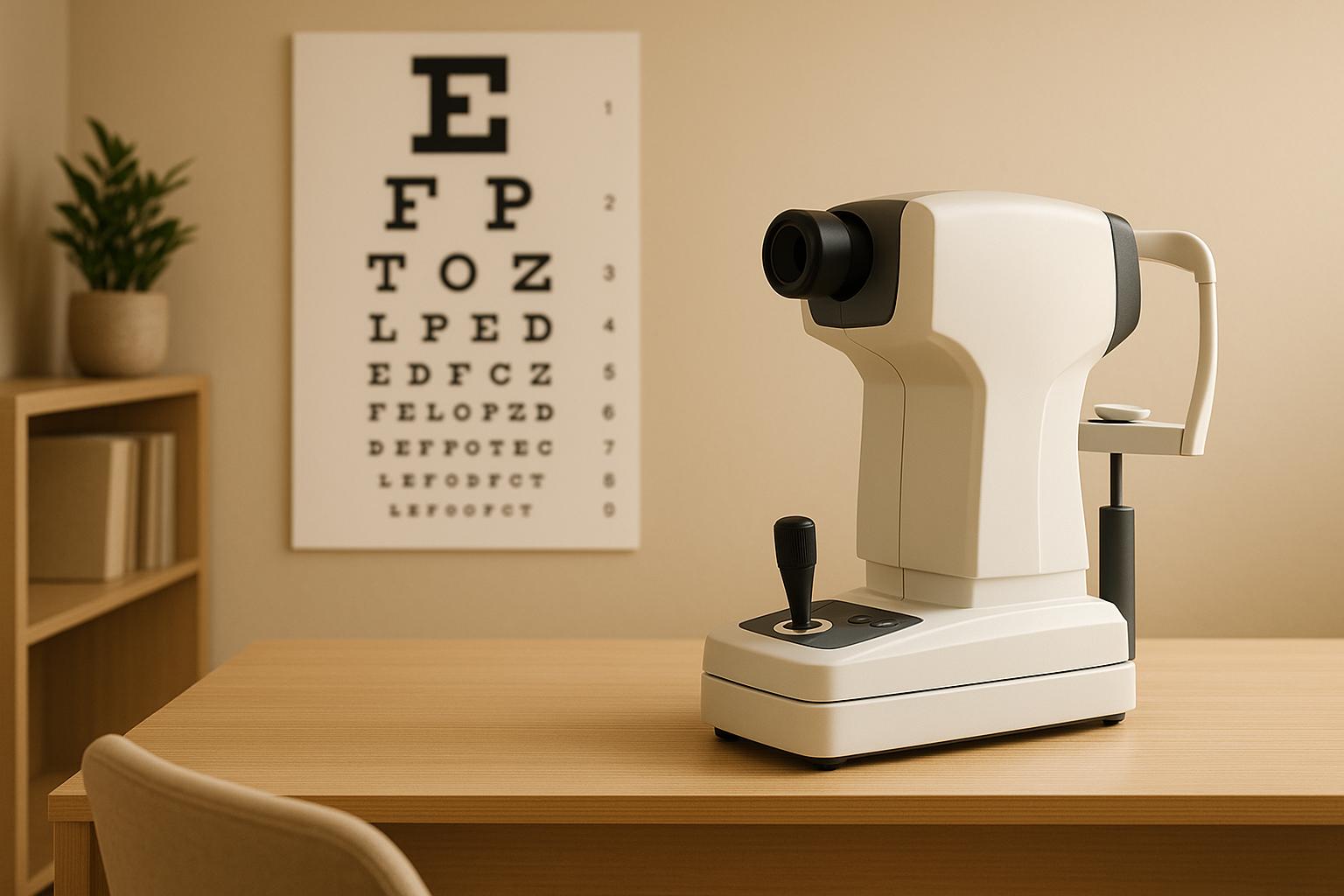
Modern technology has made screenings more precise and comfortable. Today’s diagnostic tools can identify glaucoma-related changes years before older methods could, giving you and your doctor more time to act and preserve your sight.
How Is Glaucoma Diagnosed?
Diagnosing glaucoma goes beyond just checking your eye pressure. It involves a series of specialized tests that evaluate both the pressure inside your eye and the health of your optic nerve. This is because some people with normal eye pressure can still develop glaucoma, while others with high pressure might not show any optic nerve damage. To get a full picture of your eye health, doctors rely on several key tests.
What Tests Are Used for Glaucoma Diagnosis?
- Intraocular Pressure (IOP) Measurement: A tonometer measures the pressure inside your eye. While normal pressure typically falls between 12 and 22 mmHg, this alone isn’t enough to confirm or rule out glaucoma.
- Optic Nerve Evaluation: Your doctor examines the optic disc, where the optic nerve connects to the eye, for signs of damage like cupping or thinning. Photographs are often taken to track any changes over time.
- Optical Coherence Tomography (OCT): This imaging test creates detailed cross-sectional views of the retina and optic nerve. It’s especially useful for spotting early thinning of nerve fibers, even before vision loss becomes noticeable.
- Visual Field Testing: This test maps your peripheral vision to detect blind spots or areas with reduced sensitivity. It can identify patterns of vision loss associated with glaucoma, often before you notice any symptoms.
- Gonioscopy: Using a special contact lens with mirrors, this test examines the drainage angle of your eye. It helps determine whether you have open-angle or angle-closure glaucoma by assessing how well fluid drains from the eye.
- Pachymetry: This ultrasound test measures the thickness of your cornea. Since corneal thickness can affect eye pressure readings, this information helps your doctor interpret IOP measurements more accurately.
How Does Boulder Eye Surgeons Help with Diagnosis?
At Boulder Eye Surgeons, these advanced diagnostic tools are central to their patient-first approach. They use cutting-edge technologies like Visual Field Testing and OCT to detect even the smallest changes in optic nerve structure and vision.
The team is committed to clear communication and patient education, ensuring you understand each test and its results as part of your care. Known for their professional and compassionate service, Boulder Eye Surgeons boasts a 97% patient referral rate, with many recommending them to friends and family.
sbb-itb-c87b093
What Are the Treatment Options for Glaucoma?
Managing glaucoma focuses on lowering intraocular pressure to prevent further vision loss, as treatments cannot recover vision already lost due to optic nerve damage. Early diagnosis and consistent care are key – many people with glaucoma can preserve their remaining vision for years.
Treatment plans are personalized, starting with the least invasive options and escalating as needed. Factors like the type of glaucoma, current eye pressure, overall health, and response to initial treatments help guide the approach.
What Are the Main Treatment Methods?
Eye drops are the first line of defense against glaucoma. These medications either reduce the eye’s fluid production or improve its drainage. Common types include prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors. While many patients require just one type, some may need a combination for better control.
Consistency is crucial for eye drops to work effectively. Most patients must use them daily for life, as skipping doses can allow eye pressure to increase again. Side effects might include eye irritation, changes in iris color, or, in some cases, systemic effects like altered heart rate or breathing patterns.
Laser therapies offer an alternative when eye drops are not enough or cause intolerable side effects. For open-angle glaucoma, Selective Laser Trabeculoplasty (SLT) uses laser energy to enhance fluid drainage. In cases of angle-closure glaucoma, Laser Peripheral Iridotomy creates a small opening in the iris to improve fluid flow.
Laser procedures are quick, performed in-office, and typically allow for a fast recovery – most people resume normal activities within a day or two. The effects can last for several years, although some patients may require repeat treatments.
Surgical options are considered when medications and laser treatments fail to control eye pressure. Traditional surgeries like trabeculectomy create new drainage pathways, while newer minimally invasive glaucoma surgeries (MIGS) provide less invasive alternatives with shorter recovery times. However, MIGS may be less effective for advanced cases.
Surgery carries higher risks than other treatments, including infection, bleeding, and potential vision changes. Despite these risks, surgery can be life-changing for patients with advanced glaucoma or those who cannot tolerate other treatments.
How Do Treatments Compare?
| Treatment Type | Effectiveness | Side Effects | Maintenance | Best For |
|---|---|---|---|---|
| Eye Drops | High with consistent use | Eye irritation, possible systemic effects | Daily use required | Early to moderate glaucoma, patients who can stick to a routine |
| Laser Therapy | Moderate, lasts 2-5 years | Temporary inflammation, possible pressure spike | Periodic retreatment | Patients with medication intolerance or adherence challenges |
| Traditional Surgery | High, long-lasting | Higher risk of complications | Regular follow-ups | Advanced glaucoma, failed medical or laser treatments |
| MIGS Procedures | Moderate, fewer complications | Lower risk profile | Less intensive follow-up | Mild to moderate glaucoma, often combined with cataract surgery |
The right treatment depends on your individual needs. Patients who can reliably use daily medications often start with eye drops. Those who struggle with daily routines or prefer less maintenance may benefit more from laser treatments or surgery. Your eye doctor will work with you to find the best approach for your condition and lifestyle.
How Can Glaucoma Be Managed in Daily Life?
Managing glaucoma goes beyond medical treatments – it’s about integrating healthy habits into your daily routine. Since glaucoma is a lifelong condition, staying consistent with your care plan is essential to protect your vision and minimize further damage to the optic nerve.
Sticking to your prescribed medication schedule is critical. Missing doses or inconsistent use of eye drops can lead to higher eye pressure and worsening vision over time. Alongside medication, making thoughtful lifestyle adjustments can further support your eye health.
What Lifestyle Changes Can Help?
To make eye drop use easier, tie the habit to something you already do daily, like brushing your teeth or having your morning coffee. If you’re starting treatment, tools like phone alarms or reminder apps can help you stay on track during the adjustment period.
For those using multiple eye drops, it’s important to wait at least 5 minutes between applications to allow each one to be absorbed properly. If you’re doing tasks like yard work or home repairs, wearing safety glasses can shield your eyes from potential harm.
Beyond medication, maintaining a healthy lifestyle is equally important. Regular exercise, good sleep habits, and managing stress can all contribute to better treatment outcomes. Keeping a record of your eye pressure readings and visual field test results can provide valuable insights into how well your treatment is working. This information allows you to collaborate with your doctor on any necessary changes.
Traveling with glaucoma requires a bit of planning. Always carry extra eye drops, refill prescriptions before running out, and consult your doctor about adjusting your medication schedule if you’re crossing time zones.
Finally, don’t overlook the importance of family involvement. Encouraging your relatives to prioritize their eye health can make a significant difference.
Why Is Family Screening Important?
Glaucoma often runs in families, so regular eye exams for your immediate relatives are crucial. If you have glaucoma, your parents, siblings, and children face a higher risk of developing the condition. Since glaucoma can progress silently without symptoms until significant damage occurs, early detection is key.
Encourage your family members to share their medical history with their eye care providers. This can help them establish a screening schedule tailored to their risk level. Catching glaucoma early and starting treatment before vision loss becomes severe can make a big difference in preserving sight.
Key Takeaways About Glaucoma
Understanding glaucoma is crucial for protecting your vision. This condition often develops silently, without noticeable symptoms, until significant damage has already occurred. That’s why regular eye exams are your best defense against vision loss.
To recap: glaucoma progresses quietly, but early detection, effective treatments, and lifestyle adjustments play a key role in managing the condition.
Early detection is critical. Individuals over 40, those with a family history of glaucoma, or anyone with other risk factors should prioritize comprehensive eye exams. These exams can catch glaucoma before you notice any changes in your vision, allowing treatment to begin when it’s most effective.
Once glaucoma is detected, managing it becomes the focus. Treatment often starts with eye drops, which lower eye pressure by either reducing fluid production or improving drainage. If medications aren’t enough, laser treatments like trabeculoplasty can boost the eye’s natural drainage. For more advanced cases, surgical procedures may be necessary to create new drainage pathways and better control pressure.
Consistency in treatment is essential. Missing doses of prescribed eye drops or skipping follow-up appointments can lead to further vision loss. Build treatment into your daily routine – take medications with meals or set phone reminders to stay on track.
Because glaucoma can run in families, it’s important to share your diagnosis with relatives. This helps their eye care providers determine the right screening schedule for them.
Managing glaucoma effectively involves staying on top of medications, practicing safe habits, maintaining a healthy lifestyle, and planning ahead. For example, when traveling, pack extra eye drops and ensure prescriptions are refilled in advance to avoid interruptions.
Boulder Eye Surgeons offers comprehensive glaucoma care, utilizing advanced diagnostic tools and personalized treatment plans. Their dedicated team supports patients from diagnosis through long-term management, helping you safeguard your vision for the future.
FAQs
What lifestyle changes can help manage glaucoma and protect your vision?
Supporting glaucoma treatment isn’t just about medication – certain lifestyle adjustments can play a big role in protecting your vision over time. For example, incorporating regular aerobic exercise like walking, jogging, or swimming into your routine may help reduce intraocular pressure and boost blood flow to the optic nerve. Just make sure to check with your doctor before diving into a new workout plan.
Your diet matters too. Eating plenty of leafy greens, colorful vegetables, and foods rich in omega-3 fatty acids can benefit your eye health. Beyond that, managing stress, staying smoke-free, and maintaining a healthy weight are crucial for your overall well-being and can enhance the effectiveness of your treatment. When paired with your prescribed medical care, these habits can go a long way in helping preserve your vision.
How does glaucoma progress in people with normal-tension glaucoma compared to those with high eye pressure?
Normal-tension glaucoma (NTG) behaves differently from high-pressure glaucoma. With NTG, vision loss can happen even when eye pressure stays within the normal range. This points to other factors, like reduced blood flow to the optic nerve, playing a role in its progression.
In contrast, high-pressure glaucoma is closely tied to elevated intraocular pressure (IOP), which gradually damages the optic nerve. While treatment for both conditions aims to slow their progression, managing high-pressure glaucoma focuses on lowering IOP. For NTG, however, addressing additional concerns like blood flow and the overall health of the optic nerve becomes just as important.
Why should family members of glaucoma patients get regular eye exams?
Family members of individuals with glaucoma should make regular eye exams a priority. Why? Because glaucoma has a strong hereditary link, meaning their chances of developing it are much higher. The tricky part is that glaucoma often progresses silently, showing no symptoms until vision loss becomes apparent.
Routine screenings are key to catching the condition early. Early detection means doctors can step in with treatments that help slow down or even prevent further vision loss. Taking this proactive step not only safeguards your eye health but also supports a better quality of life in the long run.