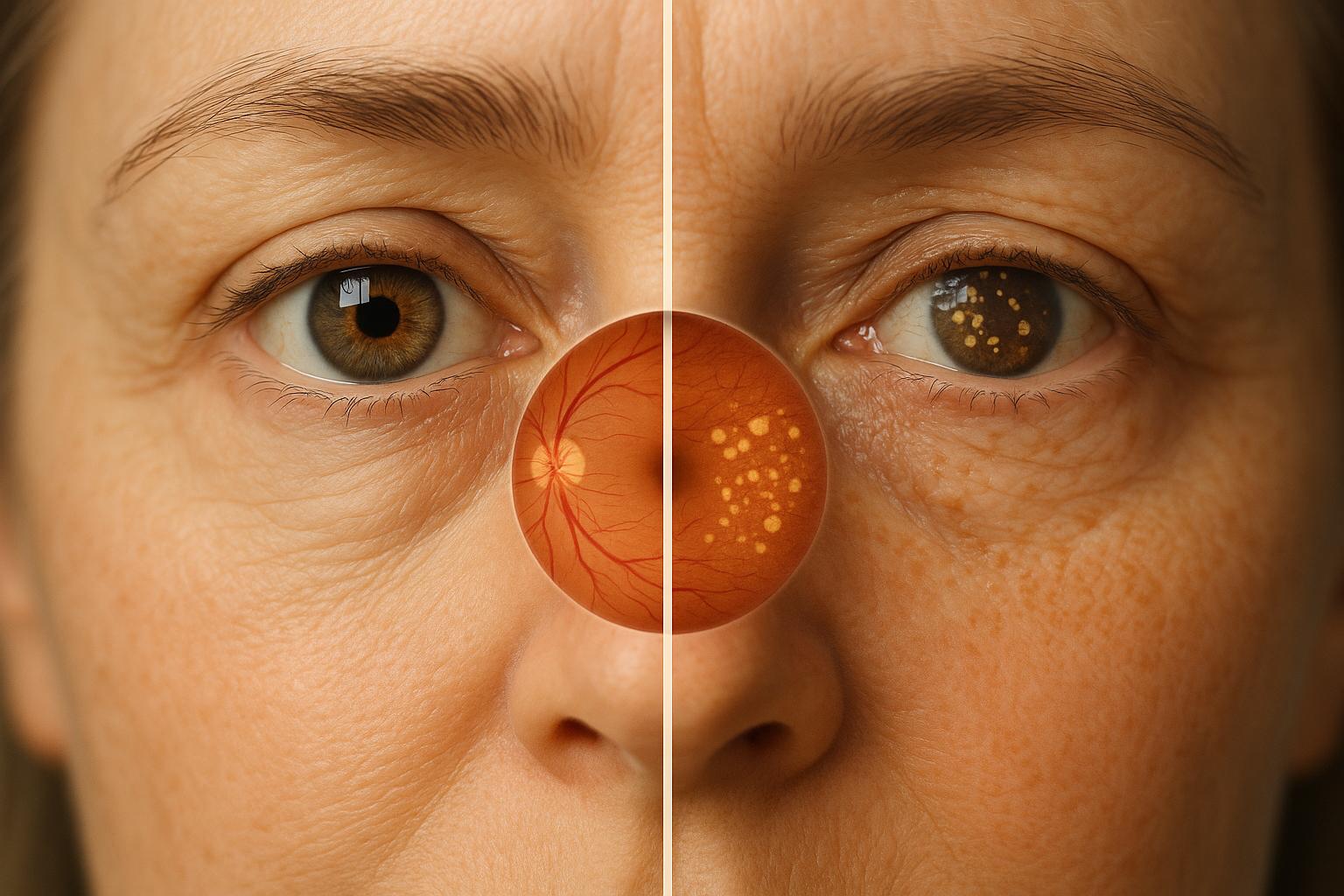
Macular degeneration, a leading cause of vision loss in adults over 65, comes in two main forms: dry and wet. Dry macular degeneration is more common, progressing slowly over years, while wet macular degeneration is less common but far more aggressive, causing severe vision loss in days or weeks. Both conditions affect central vision, making tasks like reading or recognizing faces challenging, but peripheral vision remains intact.
Key Differences:
- Dry AMD: Gradual vision changes due to thinning of the macula and drusen buildup. No cure exists, but lifestyle changes and supplements can slow progression.
- Wet AMD: Rapid vision loss caused by abnormal blood vessel growth and leakage under the retina. Anti-VEGF injections are the primary treatment, requiring urgent care.
Quick Comparison:
| Feature | Dry AMD | Wet AMD |
|---|---|---|
| Prevalence | 85–90% of cases | 10–15% of cases |
| Progression | Slow (years) | Fast (days to weeks) |
| Vision Loss | Mild to moderate | Severe and rapid |
| Cause | Drusen buildup, macula thinning | Abnormal blood vessel growth |
| Treatment | Supplements, lifestyle changes | Anti-VEGF injections, therapy |
If you notice blurred vision, wavy lines, or dark spots, seek immediate medical attention. Early detection and treatment can help manage symptoms and preserve vision.
Dry VS Wet Macular Degeneration – Age Related Macular Degeneration (AMD) Explained
Dry Macular Degeneration
Dry macular degeneration accounts for the majority of age-related macular degeneration (AMD) cases. Unlike its wet counterpart, this form progresses slowly, giving patients and doctors more time to manage the condition. It develops as the macula – the central part of the retina responsible for sharp, detailed vision – gradually thins over several years instead of deteriorating rapidly.
One hallmark of dry macular degeneration is the buildup of yellow deposits known as drusen beneath the retina. These deposits form when the retinal pigment epithelium (RPE) struggles to clear waste from photoreceptor cells. Over time, drusen disrupt the flow of oxygen and nutrients to the macula, causing it to thin and leading to a gradual loss of central vision.
Dry Macular Degeneration Symptoms
In its early stages, dry macular degeneration is often symptomless and typically detected during routine eye exams. As the condition advances to the intermediate stage, patients may notice mild central vision blurring and difficulty seeing in low-light conditions. In the late stage, symptoms become more severe. Central vision loss can significantly impact daily activities like reading, recognizing faces, or performing tasks that require precision. Some individuals may also experience blank spots in their central vision or see straight lines – such as doorframes or telephone poles – appear wavy or distorted. Despite these challenges, peripheral vision generally remains unaffected.
Causes and Risk Factors
Dry macular degeneration is primarily linked to aging, as the natural wear and tear on the macula leads to its gradual breakdown. With age, the retinal pigment epithelium becomes less effective at removing metabolic waste, allowing drusen to accumulate and damage the macula.
Age is the most prominent risk factor, with the condition primarily affecting individuals over 65. Genetics also play a role; having a family history of AMD or specific genetic variations, such as changes in the complement factor H gene, can increase susceptibility. Lifestyle factors further amplify the risk. Smoking, for instance, can triple the likelihood of developing AMD, as tobacco chemicals damage retinal blood vessels and accelerate tissue aging. Other contributors include high blood pressure, elevated cholesterol, and cardiovascular disease, all of which can reduce blood flow to the retina. Excessive sun exposure and unhealthy habits, such as poor diet and lack of exercise, may also heighten the risk. Understanding these factors emphasizes the importance of preventative care and early management.
Treatment Options for Dry Macular Degeneration
Currently, there is no cure for dry macular degeneration. However, several strategies can help slow its progression and preserve vision. One proven option is the use of AREDS2 supplements, which combine vitamin C, vitamin E, zinc, copper, lutein, and zeaxanthin. These supplements are specifically designed to slow disease progression in intermediate or advanced stages and should be taken under medical supervision.
Lifestyle changes play a crucial role in managing dry AMD. Quitting smoking is one of the most impactful steps, as it reduces further retinal damage. Adopting a diet rich in leafy greens and fish provides antioxidants and omega-3 fatty acids that support eye health. Managing cardiovascular health by controlling blood pressure and cholesterol, staying active, and wearing high-quality sunglasses to block UV rays are also important measures. Regular checkups with an eye care professional, along with the use of tools like an Amsler grid at home, can help monitor disease progression and detect any transition to wet macular degeneration.
While current treatments focus on slowing the condition rather than reversing damage, new therapies are under development. Clinical trials are exploring options like stem cell treatments and anti-inflammatory medications, which could lead to more effective solutions in the future. This ongoing research offers hope for better management of dry AMD and improved outcomes for patients.
Wet Macular Degeneration
Wet macular degeneration is a more aggressive form of age-related macular degeneration (AMD). While it accounts for only about 20% of AMD cases, it’s responsible for roughly 90% of the severe vision loss linked to the condition. Unlike the slower progression of dry AMD, wet AMD can lead to significant vision impairment in just days or weeks.
The hallmark of wet AMD is the abnormal growth of fragile blood vessels beneath the macula, a process called choroidal neovascularization. These vessels often leak blood and fluid into the retinal tissue, causing rapid damage to the cells responsible for sharp central vision. This quick progression makes wet AMD a medical urgency, requiring immediate attention.
Wet Macular Degeneration Symptoms
Symptoms of wet AMD tend to appear suddenly, highlighting the need for prompt medical care. One early sign is the distortion of straight lines – objects like doorframes or telephone poles may look bent or wavy. A dark or blurry spot often develops in the center of vision, making tasks like reading or recognizing faces difficult. Colors may appear duller, and patients may struggle to see clearly in dim lighting. These symptoms can escalate rapidly over a short period.
Causes and Risk Factors
Wet AMD frequently develops from dry AMD, as abnormal blood vessel growth beneath the retina triggers rapid vision loss. Several factors contribute to its progression. Age remains the leading non-modifiable risk factor, with the condition most commonly affecting those over 50. A family history of AMD and genetic predispositions also increase susceptibility.
Among modifiable risk factors, smoking plays a significant role in worsening abnormal blood vessel growth. Other contributors include cardiovascular problems, high blood pressure, and excessive exposure to sunlight. Addressing these modifiable risks can help reduce the likelihood of developing wet AMD.
Treatment Options for Wet Macular Degeneration
Given the aggressive nature of wet AMD, early intervention is essential. Anti-vascular endothelial growth factor (anti-VEGF) injections are the primary treatment. These medications work by halting the growth of abnormal blood vessels and reducing leakage beneath the retina. With timely treatment, some vision may be restored. Injections are typically given monthly at first, with the schedule adjusted based on the patient’s response. While mild discomfort during treatment is common, serious complications are rare.
Newer therapies, such as Faricimab (Vabysmo), offer a dual-action approach, providing additional options for patients who don’t respond well to traditional anti-VEGF treatments. In some situations, photodynamic therapy or laser treatments may still be used, though these methods are less common today. The primary goal of all treatments is to stabilize vision and prevent further loss, as restoring lost vision remains challenging. Regular follow-ups are crucial to monitor progress and adjust treatment as needed.
Research continues to focus on developing longer-lasting medications, combination therapies, and advanced delivery systems to reduce the frequency of injections while improving outcomes.
For those in Boulder, Colorado, Boulder Eye Surgeons provides specialized retina care and cutting-edge treatments for wet macular degeneration, offering personalized care with the latest technology.
Dry vs. Wet Macular Degeneration Comparison
Understanding the differences between dry and wet macular degeneration is essential for recognizing early symptoms and ensuring timely care. Each type comes with its own unique characteristics and treatment approaches, which are outlined below.
Dry AMD accounts for about 85–90% of all cases and progresses slowly over several years. On the other hand, wet AMD, which represents 10–15% of cases, can lead to severe vision loss in a matter of days or weeks .
The underlying causes of these conditions also differ. Dry AMD is marked by the buildup of drusen deposits that thin the macula over time. In contrast, wet AMD involves the growth of fragile, leaky blood vessels beneath the retina, which can quickly impair vision.
Treatment options highlight another key difference. While there is no cure for dry AMD at this time, management focuses on lifestyle changes – like quitting smoking – and the use of nutritional supplements. Research into potential treatments is ongoing. Wet AMD, however, has more established treatments, including anti-VEGF injections and, in some cases, photodynamic therapy, both of which aim to control abnormal blood vessel growth. For wet AMD, treatment is typically started within two weeks of diagnosis .
Monitoring strategies also vary. Dry AMD requires regular eye exams to track gradual changes, whereas wet AMD demands more frequent monitoring, often using tools like the Amsler grid to catch any rapid shifts in vision.
Comparison Table: Dry vs. Wet Macular Degeneration
| Feature | Dry Macular Degeneration | Wet Macular Degeneration |
|---|---|---|
| Prevalence | 85–90% of AMD cases | 10–15% of AMD cases |
| Progression | Gradual, over years | Rapid, over days to weeks |
| Vision Loss | Mild to moderate over time | Severe and rapid |
| Symptoms | Gradual blurring of central vision; difficulty in low light | Sudden vision loss; distorted lines; dark spots |
| Cause | Drusen buildup and macula thinning | Abnormal blood vessel growth and leakage |
| Treatment | Lifestyle changes, nutritional supplements | Anti-VEGF injections, photodynamic therapy |
| Monitoring | Routine eye exams | Frequent, urgent monitoring |
| Prognosis | Can remain stable for years | High risk without treatment; treatable if caught early |
These differences emphasize the importance of individualized care and timely intervention. At Boulder Eye Surgeons, advanced retina services are available to manage both forms of macular degeneration effectively.
Regular eye exams and early treatment play a critical role in preserving vision, whether you’re managing the slower progression of dry AMD or addressing the more immediate challenges of wet AMD. By staying proactive, you can make a significant difference in maintaining your quality of life.
sbb-itb-c87b093
Risk Factors and Prevention
Macular degeneration impacts millions of Americans, and understanding its risk factors is crucial for taking steps to protect your vision. Both the wet and dry forms of AMD share many of the same risks, though some may influence the disease’s progression more than others.
The main risk factors include age, smoking, genetics, cardiovascular issues, obesity, sedentary habits, low dietary antioxidants, and prolonged UV exposure. Among these, age stands out as the most critical factor. Your risk of developing AMD increases significantly after age 75, making regular eye exams essential – especially since AMD is a leading cause of vision loss in Americans over 60.
Race also plays a role. Studies show that Caucasians face a higher risk compared to African Americans or Hispanics. Knowing these factors can help guide preventive actions and reduce potential risks.
Evidence-Based Prevention Strategies
By recognizing these risks, you can take proactive measures to protect your eyesight. Simple lifestyle changes, like maintaining a balanced diet and staying active, can significantly lower your chances of developing AMD.
Quitting smoking is one of the most effective ways to reduce AMD risk. Not only does it lower your chances of developing the disease, but it can also slow its progression if you’ve already been diagnosed.
Improving your diet is another key step. Foods rich in antioxidants – like leafy greens, colorful fruits, and fish – help support retinal health. For those with intermediate or advanced AMD, AREDS2 vitamin supplements (a specific blend of vitamins and minerals) have been shown to slow the disease’s progression and are widely recommended as part of standard care.
Staying physically active, managing weight, and keeping your blood pressure and cholesterol in check benefit both your heart and your eyes.
Protecting your eyes from UV exposure is also worth considering. While research on UV light’s direct impact on AMD is mixed, wearing sunglasses with UV protection or using a brimmed hat can help reduce potential long-term damage to your macula.
Finally, regular eye exams are crucial, especially after age 50. These comprehensive check-ups can catch early signs of AMD, allowing for timely intervention and monitoring. If you have a family history of AMD or multiple risk factors, these exams become even more important.
Although these strategies can’t completely stop the progression of AMD – particularly the shift from dry to wet forms – they can make a meaningful difference. By addressing modifiable risk factors and prioritizing eye health through nutrition and lifestyle changes, you can take active steps to preserve your vision for the future.
Macular Degeneration Care at Boulder Eye Surgeons
Detecting macular degeneration early and providing specialized care can make a significant difference in preserving vision. At Boulder Eye Surgeons in Boulder, CO, patients receive expert retina care through advanced diagnostic tools and customized treatment plans.
Advanced Diagnostic Tools for Early Detection
Boulder Eye Surgeons uses cutting-edge diagnostic technology, including OCT (Optical Coherence Tomography), fundus photography, and fluorescein angiography, to identify and monitor both wet and dry macular degeneration. These high-resolution imaging techniques help detect even the smallest changes in the macula, often before noticeable vision loss occurs. Early detection like this opens the door to timely, effective treatments.
OCT, for instance, provides detailed cross-sectional images of the retina. This allows specialists to detect fluid buildup or abnormal blood vessels in wet macular degeneration, as well as signs like drusen or retinal thinning in dry macular degeneration. With this level of precision, doctors can differentiate between the two forms of the disease and determine its stage, ensuring accurate and targeted care.
Comprehensive Treatment Options for Every Patient
For patients with wet macular degeneration, Boulder Eye Surgeons offers anti-VEGF injections and other tailored treatments. These therapies are most effective when started early, highlighting the importance of quick diagnosis and intervention.
Patients with dry macular degeneration benefit from a holistic approach that includes lifestyle recommendations, nutritional guidance (such as AREDS2 vitamin supplements), and access to clinical trials when appropriate. These services are part of personalized care plans designed to address not only the medical aspects of the condition but also practical strategies to maintain the best possible quality of life.
Individualized Care Patients Can Rely On
At Boulder Eye Surgeons, patient care is deeply personal. Their mission reflects this commitment:
"Our goal is to provide professional, compassionate and customized eye care to every patient, every time. We strive to understand your needs and exceed your expectations."
This dedication means every care plan is uniquely tailored to the patient’s condition, disease stage, lifestyle, and overall health. Monitoring schedules are adjusted as needed, and treatments evolve in response to the latest advancements or changes in the patient’s condition.
Patients often express gratitude for the thoroughness and clarity of their care. As one patient, Edna B., shared:
"Dr. Nichols spent adequate time with me explaining everything thoroughly. My daughter came with me and he took the time to address her concerns and answer her questions. I am so grateful to these people for how they are addressing my problems with my eyes which involve a complex medical condition."
Coordinated Care for Better Health Outcomes
The team at Boulder Eye Surgeons works closely with other healthcare providers, including primary care physicians and specialists like endocrinologists, to manage systemic conditions – such as high blood pressure and diabetes – that can influence the progression of macular degeneration. This collaborative approach ensures all aspects of a patient’s health are considered in their treatment plan.
Beyond medical care, the practice offers education, counseling, and resources to help patients better understand their diagnosis and treatment options. They also provide training on using low-vision aids and resources to maintain independence, giving patients the tools they need to adapt to changes in their vision.
Commitment to the Latest Advances in Care
Boulder Eye Surgeons stays at the forefront of macular degeneration treatment by actively participating in medical research, professional conferences, and continuing education. By incorporating breakthroughs like dual-action therapies such as Vabysmo (Faricimab) and adopting new diagnostic techniques, they ensure patients have access to the most effective and up-to-date care options.
Whether you’re experiencing the first signs of macular degeneration or need ongoing management for an established condition, Boulder Eye Surgeons combines expertise, advanced technology, and personalized care to help preserve your vision. Their proactive approach addresses both immediate treatment needs and long-term strategies for maintaining vision health.
Conclusion
Understanding the differences between wet and dry macular degeneration is essential for protecting your vision and making informed decisions about your eye health. Dry AMD accounts for about 80% of cases and typically progresses slowly, leading to gradual vision changes. On the other hand, wet AMD, while representing only 20% of cases, is responsible for approximately 90% of severe vision loss associated with the disease. This sharp contrast underscores the importance of early detection and timely action.
As discussed earlier, managing macular degeneration effectively requires professional eye care and early intervention. Regular comprehensive eye exams, especially for those over 50, are crucial for detecting macular changes before significant vision loss occurs. Advanced diagnostic tools, like OCT imaging, can spot subtle changes in the macula, allowing for earlier and more effective treatment. Staying proactive with your eye health can make a real difference.
If you notice any changes in your central vision, seek professional evaluation immediately. The team at Boulder Eye Surgeons is equipped with cutting-edge diagnostic technology and offers personalized treatment plans to help preserve vision and maintain quality of life. With expertise in managing both wet and dry AMD, they provide the specialized care needed to address this condition.
Make regular eye exams a priority, maintain a healthy lifestyle, and act quickly if vision changes arise to safeguard your eyesight.
FAQs
What are the early signs of macular degeneration, and how can routine eye exams help detect them?
Macular degeneration often begins with subtle vision changes that can be easy to miss. Early signs might include blurred or distorted central vision, trouble seeing fine details, or needing more light for reading or close-up tasks. Some individuals may also notice straight lines appearing wavy or develop a dark, blurry spot in the center of their vision.
This is why regular eye exams are so important – they can catch macular degeneration even before symptoms become noticeable. Eye doctors use advanced tools and imaging techniques to closely examine the retina, spotting any early signs of damage or progression. Detecting the condition early means treatment can begin sooner, helping to slow vision loss and maintain your quality of life.
How can lifestyle changes and dietary supplements help manage dry macular degeneration?
Lifestyle adjustments and dietary supplements can make a big difference in managing dry macular degeneration by promoting overall eye health and potentially slowing the condition’s progression. Incorporating leafy greens, vibrant fruits, and foods rich in omega-3 fatty acids into your diet can supply key nutrients like lutein, zeaxanthin, and antioxidants, which help protect the retina from harm.
Doctors may also suggest specific supplements based on the findings of the Age-Related Eye Disease Study (AREDS). These typically include vitamins C and E, zinc, and copper. Beyond diet, adopting healthy habits – such as quitting smoking, controlling chronic conditions like high blood pressure, and wearing UV-blocking sunglasses – can further support your eye health and reduce risks linked to macular degeneration.
It’s important to consult with a qualified eye care professional to create a plan tailored to your specific needs. If you’re looking for personalized care, Boulder Eye Surgeons provides advanced retina services for patients in Boulder, CO, and nearby areas.
What are the latest treatment advancements for wet macular degeneration, and how do they benefit patients?
Recent progress in treating wet macular degeneration is centered on enhancing vision outcomes while cutting down the number of treatments patients need. Anti-VEGF injections continue to be the primary approach, effectively slowing disease progression and, in many cases, even improving vision. To make life easier for patients, newer options like extended-release formulations and implantable devices are being developed. These advancements aim to reduce how often injections are needed, offering more convenience.
In addition, cutting-edge therapies like gene therapy and complement inhibitors are making waves in clinical trials. These treatments target the root causes of the disease, potentially delivering longer-lasting effects and improving patients’ overall quality of life. If you’re considering treatment options, it’s essential to consult a specialist to determine what works best for your specific condition.